I’m a planner and it drives me nuts that I have no idea when this baby is going to decide to make their entrance into this world. Over the past few days knowing I only have a few more weeks to go, it has been on my mind constantly. It doesn’t help that I had my son a week early at 39 weeks, so it’s hard not to compare…but that doesn’t mean I won’t go late this time :/.
I thought it would be fun to share a list of natural ways to induce labor. Even though I’m not sure if I believe any of these, because I think ultimately the baby will come when he or she is ready, you never know! And if you’ve been in this situation you know you’re willing to try anything!
Please keep in mind that its not recommended to try some of these natural ways to induce labor before you estimated due date and to consult with your doctor or midwife before hand.
- Walking – Walking and consistent exercise are said to help strengthen your body to prepare for an easier and faster labor. Walking often in the last few weeks can help get things going!
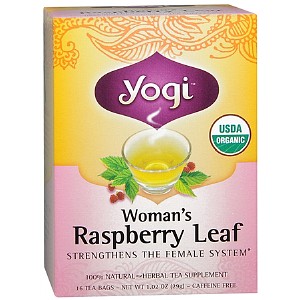
- Red Raspberry Leaf Tea – The red raspberry leaf is a uterine tonic and while it’s not supposed to actually induce labor, it is known to help prepare your body and help the onset of labor on time and help your cervix dilate faster (not too early or not late). Read more about this here.
- Massage – Induction massage is recommended on or after your due date. The massage therapists (who should be experienced in induction massage) work on acupressure points which are normally avoided during pregnancy, which can trigger labor. As with normal massage, induction massage helps to relax and calm your body, easing tension.
- Acupuncture – Acupuncture has been used successfully for thousands of years to induce women who are over-due in their pregnancy. Some acupuncture therapists don’t recommend that you get a treatment until your estimated due date, unless otherwise advised by your doctor or midwife because it can induce labor as soon as 6-48 hours after the treatment.
- Chiropractor – If you can find a chiropractor trained on the Webster method it is supposed to help align and open your pelvis which can help your baby get into an optimal birthing position.
- Spicy food – An old wive’s tale says that eating spicy food can help induce labor. I don’t know how true this one is but I did eat spicy tacos the night I went into labor with my son at 39 weeks…coincidence? Maybe. This pregnancy I also learned about an eggplant parmesan recipe from a restaurant that supposedly induces labor. Here are all the babies born after their mamas ate their eggplant parm. Find the recipe for Scalini’s Eggplant Parmesan Recipe here.
- Sex – It’s funny that the same act that got you into this pregnancy can also help the baby come out :).
- Evening Primose Oil – This is an herb that many midwives swear by in the later stages of pregnancy. Starting at about 36 weeks taking 1,000-2,000 mg orally and after 38 weeks inserting an oil capsule vaginally can help induce labor and also help speed up dilation. (Please consult with your doctor or midwife before you try an herbal supplement.)
- Pedicure/Foot Reflexology – Who cares if this one really works or not…go treat yourself and relax. If you happen to go into labor, awesome :).
- Eat some dates – This is a new one to me but I’ve read that studies have been done to prove that eating dates late in pregnancy (last four weeks) can help you go into spontaneous labor and help you dilate quicker. Hey, why not?
Who knows if any of these natural ways to induce labor really work but they are worth a try and they beat medical induction! Please share any other proven natural ways to induce labor in the comments section.
If you’re not already, please be awesome and follow me on Facebook, Instagram, Pinterest, and Twitter! Thank you :).